When your child’s cheeks burn and you feel a flush radiating across their forehead, the first question arises: “Is that a fever?” Swiftly, parents often resort to the normal temp under the arm check, simple, noninvasive, and widely trusted for newborns. But does ease equate with accuracy? And if results seem dubious, what then?
We must first understand what fever truly signifies, how precise readings are obtained, and which ranges qualify as “normal” depending on the method used. Because it can be a mild sniffle or something more ominous, the technique matters, perhaps more than you imagine.
Fever: Not the Villain, but a Messenger
Be clear: fever isn’t an illness; it’s an immune response. If combating viral invaders, bacterial intruders, or reacting post-immunization, the body’s thermostat gets reset. But alarm bells? Not always warranted. Most fevers self-resolve within 72 hours; no intervention needed.
The key lies in understanding how you take the temperature, what defines “normal,” and discerning when escalation is required.
Axillary Temperature: Comfort with Caveats
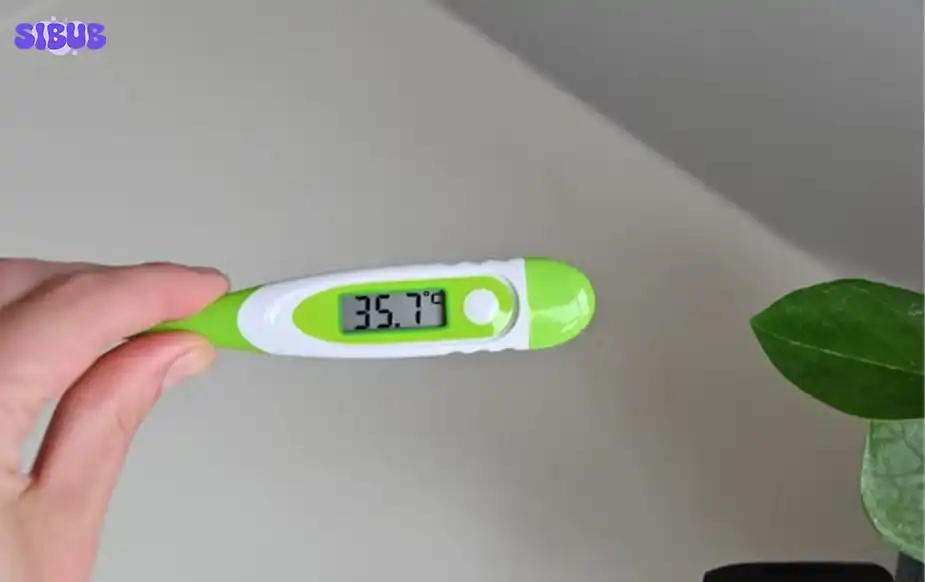
A normal temp under the arm is typically between 36.5 °C and 37.2 °C (97.8 °F–99 °F). Yet note, axillary readings often trail behind core body temperature, especially in infants. Quick, yes. Accurate? Less so.
When it’s useful:
- Ideal for newborn screenings
- A fast, first-line check
- But if your child seems ill despite a “normal” axillary reading, insist on a more accurate method.

Visit: How to Play Charades: Rules for Kids
Tip: Age Dictates the Method
The thermometer you choose should follow your child’s age. Begin here for immediate clarity:
- 0–2 years: Rectal reigns supreme; armpit as an alternative
- 2–5 years: Rectal remains top-tier; ear or axillary also acceptable
- 5+ years: Oral excels; ear or axillary are viable next picks
Thus, if you’re curious about a normal ear temperature, know that reliability increases only once kids are past two years.
Ear Thermometry: Swift, But Slippery
Aim, press, beep, it sounds like the ideal method. But ear readings (tympanic) can mislead, yielding values lower than reality if probe hygiene falters or placement is off. The expected normal ear temp lands between 35.8 °C and 38 °C (96.4 °F–100.4 °F).
Guidelines for use:
- Always swap in a clean probe tip
- Gently pull the ear back to open the canal for accuracy
- If numbers seem low but your child feels hot or uneasy, cross-verify with oral or rectal measures
Remember: ear thermometry shouldn’t be the only strategy for infants.
Rectal Temperatures: The Nonpareil Standard
For absolute precision, in infants especially, rectal temperature measurement is the gold standard. A normal rectal temperature lies between 36.6 °C and 38 °C (97.9 °F–100.4 °F). Anything above 38 °C (100.4 °F)? That’s fever territory.
In newborns, a rectal reading crossing that threshold demands physician attention immediately.
“Rectal thermometry remains the most reliable for detecting fever in infants under 3 months of age” (El‑Radhi, 2008).
Discover: How to Play Poker: Simple Rules for Beginners
Thermometer Types: A Breakdown
A digital thermometer is your safest, most versatile friend; unbreakable, fast, easy to read, and clean. But keep it hygienic: never swap mouth for bum use.
- Digital / electronic: can be used orally or rectally
- Non-contact infrared: fast, yet prone to drift based on sweat, environment, and headgear
- Mercury: avoid entirely, fragile and toxic
- Fever strips/pacifier thermometers: inaccurate; disregard
Choose wisely.
How to Properly Take Each Temperature
Rectal (infants, most accurate)
- Wash the thermometer with soap and rinse
- Lubricate the tip with petroleum jelly
- Lay the baby on their back, knees bent
- Gently insert ~2.5 cm (1″), hold
- Wait for the beep, extract, and read
- Clean once more afterwards
Oral (kids 5 and up)
- Sanitize thermometer
- Place under tongue, off to one side
- Instruct the child to close their mouth
- Wait ~1 minute until beep
- Read and clean
Axillary (all ages, quick)
- Clean thermometer
- Position the tip in the center of the underarm
- Hold the arm snugly in place
- Beep, read, wash again
- If no fever appears yet child is ill-looking, try rectal measurement
Tympanic (2+ years)
- Use a clean, single-use tip
- Tug the ear gently to straighten the canal
- Insert snugly, press the button for one second
- Remove, read
- If underwhelming but child feels unwell, confirm with rectal or oral
Temporal (forehead)
- Hold according to the manufacturer’s instructions
- Note that sweat, direct sun, humidity, and forehead coverings can skew results, unreliable if conditions aren’t ideal

Learn More: 23 Children’s Games for Valentine’s Day – Fun, Sweet & Easy Ideas
Normal Temperature Ranges by Method
| Method | Normal Range °C (°F) |
| Rectal | 36.6 – 38.0 (97.9 – 100.4) |
| Oral | 35.5 – 37.2 (95.9 – 99.0) |
| Axillary | 36.5 – 37.2 (97.8 – 99.0) |
| Ear | 35.8 – 38.0 (96.4 – 100.4) |
Yes, even within “normal,” those numbers weave in and out depending on when and how the reading was taken.
Fever Thresholds Simplified
A temperature above 37.9 °C (100.4 °F) typically qualifies as fever, but always tie it back to the measurement method. More crucial than the reading? How your child appears and behaves. A mild illness might spike a high fever; a severe bacterial infection might not.
At-Home Care: Start With Comfort
A fever isn’t always a crisis. But treat the child, not the thermometer.
- Encourage fluids (water, breastmilk, formula)
- Dress lightly, but not scantily; shivering can raise internal temperature
- Avoid excessive layering or stripping clothes
Medication: Not Always Necessary
If aches, pains, or crankiness arise, then perhaps consider medication. But don’t treat fever simply because it’s high.
Options:
- Acetaminophen (e.g., Tylenol®, Tempra®): safe, effective
- Ibuprofen (e.g., Advil®, Motrin®): best only if child is drinking; not for under 6 months
- Aspirin: off-limits under 18; risk of Reye’s syndrome
- You may alternate acetaminophen and ibuprofen, track times and doses meticulously
Never exceed weight-based dosage. Ibuprofen demands hydration. Aspirin is a no when dealing with flu-like or viral contexts.
Red-Flag Symptoms: When to Call the Doctor
Swift medical attention is essential if your child:
- Is under 3 months with any fever
- It is under 6 months and seems off
- Experiences fever beyond 72 hours
- Is unusually irritable, lethargic, or unresponsive
- Exhibits breathing difficulty or persistent cough
- Has rash, vomiting, diarrhea, and a stiff neck
- Drinks poorly or reduces urine output
- Recently traveled abroad
- Has had a febrile seizure
- Shows pale, cold, or patchy-textured skin
Parent Pitfalls: What to Avoid
- Relying on skin-touch over thermometer data
- Equating fever height with illness severity
- Ignoring worrying symptoms despite “mild” fever
- Failing to sanitize the thermometer
- Using ear probes on infants under 6 months
- Swapping rectal for oral thermometers, label them!
Explore: How to Play Hearts: Simple Card Game Rules to Learn
Ultimately,
A normal temp under the arm offers quick reassurance, but shouldn’t be the endpoint. Your child’s age, symptoms, and behavior guide your choice of method. A digital thermometer should be in your toolkit.
Learn each method, and practice clean technique. And remember: the real sign of illness isn’t the number on the display, it’s the signs your child shows, the fluids they take, their energy, their breathing.
Fever is a clue. You hold the bigger picture.
